
:max_bytes(150000):strip_icc()/degrees-of-burns-1298906_v2-b34a363d24824c8b935448fe774a753d.png)
Any blisters often break because of the fragile thin layer of skin involved. In some cases, these may develop small blisters that appear after a couple of days. The most common type of burn is a first degree burn. This is important in providing the receiving hospital with the involvement of the burns, giving staff time to prepare for the patient. When determining the extent of burns, remember that the patient may have a combination of second and third degree burns. Understanding this is important to ensure an accurate determination of burned areas. This can lead to scald burns on their heads and upper torso burns to the head area of a child will result in a greater surface area of a child being injured when compared to the head of an adult. Children's burns often happen when they pull a hot liquid, such as coffee or a pan of hot liquid, onto themselves. It is important to remember that there is a difference between the surface area of an adult and that of an infant/child specifically, a child’s head is larger and their legs smaller compared to adults.(Interestingly, this difference in children changes their center of gravity and is why they fall over easier than older people.) When it comes to burns and children, keep in mind that youngsters are always reaching and pulling things. A rule of thumb is that the patient's palm represents 1 percent of their body surface area. As you can see from the graphic below, the body surface is broken down into areas representing 9 percent or multiples. The easiest way to determine the amount of area burned is by using the "Rule of Nines." This formula is easy to remember and accurate. When treating burn patients, the provider should be able to determine the extent of the burned areas. It takes approximately 24 hours for a burn to fully "declare" itself regarding its severity.

One of the cardinal rules when working with burn patients is to never underestimate the severity of a burn. Be careful when cooling the burn that you do not cool the patient into a hypothermia state. It is important to keep the burn victim warm as their thermoregulation may be disrupted. Do not use a towel since the fiber can stick in the wound and be painful to remove. If the burn covers more than 30 percent of the total body surface area, you may have swelling in areas remote from the burn due to fluid shifts, so remove everything that might be constrictive.Īfter cooling the burn with water, cover the area with a clean dressing. Loosen or remove tight clothing, jewelry and boots before swelling occurs. Remove burned clothing, metal from belt buckles, etc, as these things can continue to burn if they retain heat. Do not use ice on burns as it may decrease the blood supply to the area and may actually make the burn worse.
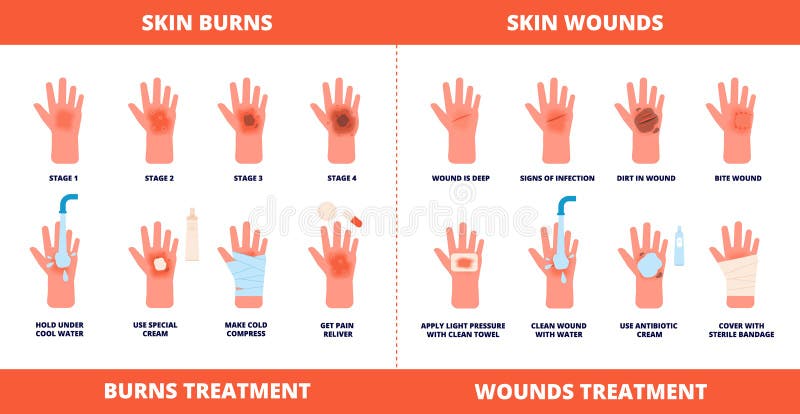
This can keep the heat trapped and further increase the burning process.Ĭool the burn immediately with cool water to reduce the skin temperature, stop the burning process, numb the pain and prevent or reduce swelling.

For the first responders, it is common to arrive on scene and find the patient wrapped in blankets or some other type of cover. The first rule for managing burn patients is to stop the burning process. Remember 2 Things: Caring for airway burns and managing swelling


 0 kommentar(er)
0 kommentar(er)
